Vorasidenib reimbursement progress (Australia)
Servier has recently made a submission to the Pharmaceutical Benefits Advisory Committee (PBAC) to place vorasidenib on the Pharmaceutical Benefits Scheme (PBS).
The PBS is a government program to make medicines more affordable to help ensure that everyone who needs medicine can access it, no matter their financial situation.
The PBAC meet four times a year to assess whether medicines are good value for money, to be listed on the PBS. This process can take up to 17 weeks.
We will keep you updated on the progress of this application.
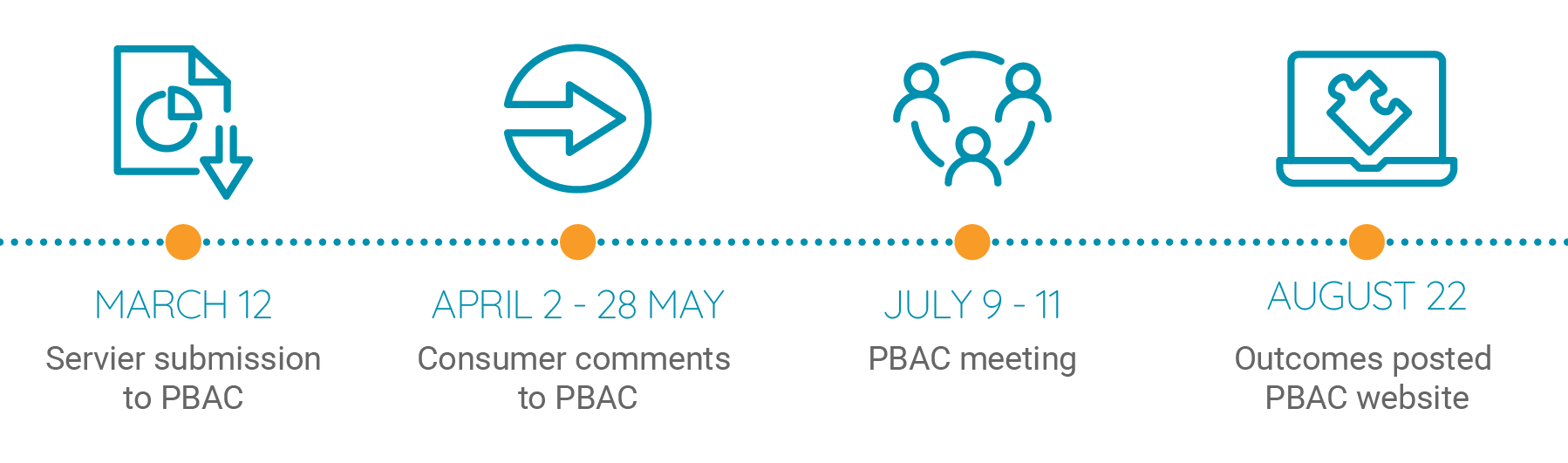
The PBAC invites anyone with an interest in a particular treatment or condition, to provide input into the assessment process. Sharing lived experience and insights helps the PBAC to better understand the impact that access to medicine can make to a patient or carers life.
Consumer comments are open until 28th May in the lead up to the PBAC meeting and submissions can be made here.
Why have I been prescribed vorasidenib?
- Vorasidenib is used to treat certain types of brain cancers which have a mutation in the cancer genes that code for IDH1 or IDH2 proteins.
- You have been prescribed vorasidenib because testing of your tumour tissue has identified either an IDH1 or IDH2 mutation.
Is vorasidenib approved for use in Australia and New Zealand?
- Vorasidenib is approved for use in Australia by the Therapeutic Goods Administration (TGA), following surgery in people 12 years or older with specific brain cancers with a IDH1 or IDH2 mutation.
- Vorasidenib has not yet been submitted to MEDSAFE and is currently not approved for use in New Zealand.
How does vorasidenib work?
- The IDH1 and IDH2 proteins play an important role in making energy for cells.
- When the IDH1 gene or IDH2 gene is mutated, the IDH1 or IDH2 protein is changed and does not function properly. This results in changes in the cell that can lead to the development of cancer.
- Vorasidenib blocks the mutated IDH1 or IDH2 and helps to slow or delay the cancer growth.
Below is a summary of some information about vorasidenib. For more information, please read through the Consumer Medicine Information and also speak to your healthcare professional.
What should I know before I start treatment
There are some people who should not take vorasidenib. Please read the list below. If you think any of these situations apply to you or you have any questions, please see your doctor.
Do not use vorasidenib if:
- you are allergic to vorasidenib or any of the other ingredients of the tablet (click here for more information)
- you are pregnant or plan to become pregnant (vorasidenib may be harmful to your unborn baby)
- you have a rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption, as vorasidenib contains lactose
- you are under 12 years of age
Vorasidenib is processed by your liver, and you need to have good liver function to receive the usual dose of vorasidenib.
- Blood tests including liver function tests (ALT, AST and total bilirubin) must be monitored before starting vorasidenib, every two weeks for the first 2 months of treatment and then monthly throughout the duration of the treatment or as clinically indicated.
- The dose of vorasidenib may be reduced, stopped temporarily or permanently according to your liver function test results.
Check with your doctor if:
- you have severe liver problems as you may be treated with vorasidenib only after careful risk/benefit assessment and you will need to be closely monitored
- you have kidney problems
- take any medicines for any other condition
- you might be pregnant or are planning to have a baby (please see further information below)
- you are breastfeeding or intend to breastfeed
- if you or your partner use a hormonal contraceptive
- you are under 12 years old or over 65 years old
Are there any interactions with other medicines I should know about?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop. This is because they may reduce how well vorasidenib works or increase the risk of side effects, or vorasidenib may affect the way these other medicines work.
In particular, tell your doctor if you are taking any of the following medications:
Medicines that may increase the effect of vorasidenib include:
- fluvoxamine (medicine used for depression)
- ciprofloxacin (antibiotics used for bacterial infections)
Medicines that may reduce the effect of vorasidenib include:
- phenytoin (medicine used for epilepsy)
- rifampicin (antibiotics used for bacterial infections)
Vorasidenib may decrease the effect of these medications:
- alfentanil, midazolam (medicine used for anaesthesia in surgery)
- carbamazepine (medicine used for epilepsy)
- ciclosporin, everolimus, sirolimus, tacrolimus (medicines used after organ transplants known as immunosuppressants)
- fentanyl (medicine used for severe pain)
- ifosfamide, ibrutinib (medicines used for cancer)
- tamoxifen (medicine used to prevent breast cancer)
- darunavir (medicine used for HIV)
- hormonal contraceptives
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect vorasidenib.
What are the possible side effects?
All medicines can have side effects. Some side effects may need medical attention.
Ask your doctor or pharmacist if you have any further questions about side effects after reading the below information.
| Serious side effects | What to do |
|---|---|
| Very common (may affect more than 1 in 10 people): • Increased amount of liver enzymes in blood (ALT, AST, GTT). Symptoms may include yellowing of the skin or the white part of your eyes (jaundice), dark ‘tea-coloured’ urine, loss of appetite, pain on the upper right side of your stomach area, feeling very weak or tired. | Call your doctor straight away or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
| Less serious side effects | What to do |
|---|---|
| Very common (may affect more than 1 in 10 people): • Diarrhoea • Decreased count of blood platelets that can cause bleeding and bruising Common (may affect up to 1 in 10 people): • Increased blood sugar levels (hyperglycaemia) • Decreased appetite • Low blood phosphate levels that can cause confusion or muscle weakness (hypophosphataemia) | Speak to your doctor or pharmacist if you have any of these less serious side effects and they worry you or if you do not understand something in this list. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to Servier or to the Therapeutic Goods Administration. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
How do I take vorasidenib?
Always take this medicine exactly as your doctor has instructed. Check with your doctor if you are unsure.
The recommended dose is:
- 40 mg orally once daily if you weigh at least 40 kg
- 20 mg orally once daily if you weigh less than 40 kg

Swallowed whole with a glass of water

Take once daily at about the same time each day

Do not eat 2hrs before or 1hr after taking vorasidenib

Do not split, crush or chew the tablets
Do not swallow the silica gel desiccant found in the bottle. The silica gel desiccant helps protect the tablets from moisture.
If you vomit after taking your usual dose, do not take additional tablets. Take your next dose as usual on the following day.
If you forget to take vorasidenib:
- if a dose is missed or not taken at the usual time (within 6 hours), take the tablets as soon as possible
- if you missed by more than 6 hours, you should skip the tablets and take the next dose as usual on the following day
If you take too much vorasidenib:
If you think that you have used too much vorasidenib, you may need urgent medical attention.
You should immediately do one of the following:
- phone the Poisons Information Centre (by calling 13 11 26), or
- contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do one of the above even if there are no signs of discomfort or poisoning.
Do not stop using vorasidenib suddenly without consulting your doctor.
What else should I know while taking vorasidenib?
Regular Tests
You will be monitored closely by your doctor before and during treatment with vorasidenib.
- You will need to have regular blood tests of your liver function, including ALT, AST and total bilirubin before starting vorasidenib, every 2 weeks during the first 2 months of treatment and then monthly throughout the duration of the treatment or as clinically indicated.
- The dose of vorasidenib may be reduced, vorasidenib may be stopped temporarily or permanently according to your liver function test results.
- Call your doctor straight away or go straight to the Emergency Department if you experience any serious side effects.
- Remind any doctor, dentist or pharmacist you visit that you are using vorasidenib.
Monitoring
- Your doctor will monitor your tumour growth with MRI scans to check that it is not growing too quickly. These scans will likely be more frequent initially, and may become less frequent over time.
Family planning
- It is important to tell your doctor if you are pregnant or intend to become pregnant, or if you are breastfeeding or intend to breastfeed.
- Vorasidenib is not recommended for use during pregnancy as it may harm the unborn baby. People of child-bearing age should have a pregnancy test prior to starting treatment with vorasidenib and should avoid becoming pregnant during therapy. (See below ‘Contraception in women and men’.)
- If you are pregnant, think you might be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine. Contact your doctor immediately if you become pregnant whilst taking vorasidenib.
- As vorasidenib may affect an unborn developing baby, it is important for women not to become pregnant for at least 3 months after treatment discontinuation.
Contraception in women and men
- People who might become pregnant, and people who have partners who might become pregnant, should use effective contraception during treatment with vorasidenib and for at least 3 months after the last dose.
- Vorasidenib may stop hormonal contraceptives from working properly. If you or your partner use a hormonal contraceptive (e.g. birth control pills, or contraceptive patches or implants), you should also use a barrier method (e.g. condoms or a diaphragm) to avoid pregnancy. Talk to your doctor about the right contraceptive method for you.
Breastfeeding
- It is not known if vorasidenib passes into breast milk. Do not breastfeed your baby during treatment with vorasidenib and for at least 2 months after the last dose.
Fertility
- It is not known if vorasidenib affects fertility. If you are concerned about your fertility whilst taking vorasidenib talk to your doctor.
Driving or using machines
- This medicine is not likely to affect your ability to drive or use any tools or machines, but if you feel unwell after taking vorasidenib, do not drive or use any tools or machines until you feel well again.
Drinking alcohol
- Tell your doctor if you drink alcohol.
- Drinking alcohol could worsen certain side effects that you may have with vorasidenib.
Looking after your medicine
- Follow the instructions in the carton on how to take care of your medicine properly.
- Store it in a cool dry place below 30°C. Do not store it in the refrigerator, bathroom, near a sink, in the car, or on windowsills.
- Keep the bottle tightly closed.
- Keep out of reach of children.
When to discard your medicine
- Once opened, vorasidenib should be used within 60 days.
- Do not use this medicine after the expiry date which is printed on the bottle label and box after the expiry date.
- The expiry date is the last day of the printed month.
Getting rid of any unwanted medicine
If you no longer need to use vorasidenib or it is out of date, please take it to the dispensing pharmacy for safe disposal.
