You may already have a good understanding of what glioma is, but if you want to learn more about the disease, or help your family or friends understand, the information in this section aims to provide a broad overview of the disease and the treatment journey.
Adult-type diffuse glioma is a cancer that arises from certain types of brain cells. Cancer cells form when cells in the body no longer behave normally due to mutations. These cells generally grow at a fast rate and form tumours. Astrocytoma, oligodendroglioma, and glioblastoma are all different types of gliomas. They can hinder normal brain function and cause various symptoms.
What are the common symptoms of glioma?
Symptoms of glioma can vary from patient to patient and can be affected by tumour type and location.
Both before and after a glioma diagnosis, patients may experience:

Changes in mental function

Seizures

Speech difficulties

New weakness or numbness in one or more body parts
(e.g. fingers, an entire leg, one side of the face)

Headache

Nausea

Vomiting
Glioma diagnosis and management
Both the size and location of your tumour(s) will have an impact on whether the tumour can be removed by your neurosurgeon, and how much of it can be removed. While there is still a chance that the tumour will grow again after a surgery, reducing the size of the tumour is often the first treatment approach.
The surgery on a brain tumour is often called a resection. If all of the tumour is able to be removed it is called a total or complete resection. Sometimes only a part of the tumour is able to be removed, because of the risk of damaging surrounding healthy parts of your brain, this is called a sub-total or incomplete resection. The tumour that is remaining after surgery is often called residual disease.
If your tumour cannot be removed entirely, you may have a small sample of it removed to be analysed (i.e. biopsy). The sample will be sent to a pathology lab where pathologists will determine what kind of tumour it is. Even though it cannot be removed, the report from the lab will help you and your doctor choose the next step on your journey. If a biopsy cannot be done, your doctor will use your brain scans to help you determine your next course of action.
Following a resection, biopsy, or brain scan, you and your doctors will be able to decide what the the best approach to treatment will be moving forward.

Your glioma was found to have an IDH mutation, which makes you eligible for treatment with vorasidenib.
- Your tumour might also have other mutations, knowing these can give you and your doctor clues about how aggressive the cancer might be.
- Knowing about the other mutations found by the pathologist might give you options for other treatments in the future, through clinical trials or new treatments that emerge.
Understanding how gliomas are classified
Understanding The Updated 2021 WHO glioma classifications
Before 2016, gliomas were classified according to what the cells looked like under a microscope, which could be interpreted differently from one healthcare provider to another.
With advancements in our understanding of mutations, the World Health Organization (WHO) updated the classification system in 2021, which created a more accurate way to categorise brain tumours.
Today, the standard practice for classifying gliomas is to obtain a genetic profile. This has created a database of information about the types of gliomas and their associated mutations.
The two main categories used are mutations in the IDH gene and 1p/19q-codeleted chromosomes.
WHO classification now has 3 categories for classifying adult-type diffuse gliomas:
| Type of glioma | Associated mutations | Grade |
|---|---|---|
| Astrocytoma | IDH-mutant | 2, 3, 4 |
| Oligodendroglioma | IDH-mutant, and 1p/19q-codeleted chromosomes | 2, 3 |
| Glioblastoma | IDH–wild-type (non-mutated IDH) | 4 |
The grading of a tumour provides information about how far advanced it is and how quickly it is likely to grow. A tumour grade of 0 is the least advanced, and a tumour grade of 4 is the most advanced. Gliomas that are grade 2 or less are considered to be low grade gliomas. Grade 3 or 4 gliomas are considered to be high grade gliomas.
The power of knowledge
By seeking information about glioma, you are arming yourself and your loved ones with the power to advocate for your own health. Understanding glioma, how it can be treated, and knowing what mutations your glioma may have will help you navigate this diagnosis.
How do mutations impact glioma
Different genetic mutations affect glioma in various ways. Identifying mutations can help you and your doctor understand your symptoms, how your tumour is likely to behave over time, and make decisions about treatment for your glioma.
Testing for an IDH mutation in all patients with glioma is essential based on the most current guidelines. After a brain scan, your tumour(s) may have been partially or completely removed, or a biopsy may have been performed. In either scenario, the tumour tissue will be sent to a lab for analysis. The lab will test the tissue for mutations like IDH1 and IDH2. Your glioma will also be tested for other mutations, such as a
1p/19q-codeletion, ATRX, and CDKN2A/B.
~400 people are diagnosed with an IDH-mutant glioma in Australia and New Zealand every year. (AIHW)
Newly diagnosed astrocytoma and oligodendroglioma in Australia (2019)
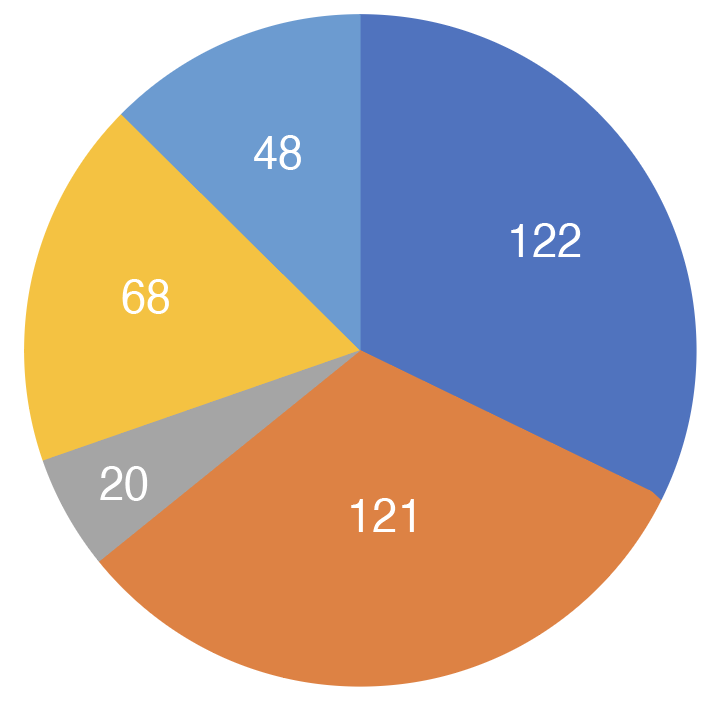
Astrocytoma, IDH-mutant, grade 2 & Astrocytoma, NOS
Astrocytoma, IDH-mutant, grade 3
Astrocytoma, IDH-mutant, grade 4
Oligodendroglioma, IDH-mutant and 1p/19q-codeleted, grade 2 & Oligodendroglioma, NOS
Oligodendroglioma, IDH-mutant and 1p/19q-codeleted, grade 3
Source: Australian Institute of Health and Welfare
How mutations in glioma may affect my prognosis
Your prognosis is an estimate of how your doctor believes your disease will behave over time and what the outcome will be. If your glioma has an IDH mutation, the outlook is usually more favorable than if it does not have an IDH mutation. Make sure you discuss with your provider what your glioma’s mutational status means for you.

You are your most powerful ally
Advocating for yourself will help you and your doctor meet your treatment goals. You can help guide your treatment journey with the glioma knowledge you’ve learned and have a productive discussion with your doctor.
Working with your healthcare team
Communication about expectations is encouraged from both sides
You and your healthcare team will create a treatment plan tailored to your needs and preferences. The treatment plan will include if and when treatment should start, what type of treatment is right for you, and how often your follow-up appointments will be. Be sure to communicate your treatment goals with your healthcare team so they can build them into your plan.
Follow-up appointments, including brain scans, are a vital part of your treatment plan. Work with your healthcare team to follow their recommended appointment schedule as closely as possible.
What happens after your diagnosis?
A glioma diagnosis can be overwhelming and may require you to make some adjustments in your life.
Some people living with glioma are able to continue taking care of their children, going to work, exercising, and going to school after receiving their diagnosis. Be mindful that there will be extra planning involved, and some new limitations.
You may have to go to a treatment center for some therapies, such as chemotherapy infusions and radiation. Recovery therapies that may be performed outside the home include occupational therapy and speech therapy. Someone else may need to drive you to and from the sessions. Start making a plan for how you will get to and from your appointments.
What can I expect from my glioma treatment?
You and your doctor will develop a treatment plan that is personalised to you. Here are some of the options that are available. Note that some may be used in combination with each other.
| Treatment options | Treatment goal | |
|---|---|---|
| Surgery (resection) | If your tumour(s) can be removed and you are healthy enough to have surgery, your doctor may recommend a total or partial resection. If your tumour grows back, your may be suitable for a repeat resection | Reduce pressure in the brain, stop progression, and relieve symptoms |
| Observation period (“watch and wait”) | In some cases, delaying treatment gives you and your doctor more time to evaluate your disease | Reduce the amount of time you may experience possible side effects from treatment |
| Radiation therapy | A type of cancer treatment that uses rays to destroy cancer cells | Kill the remaining cancer cells after a resection |
| Chemotherapy | Chemotherapy for gliomas can be given as infusions and as pills taken by mouth | Kill the remaining cancer cells after a resection |
| Clinical trials | Clinical trials study new ways of preventing, diagnosing or treating conditions and diseases. | Gain access to cutting-edge treatments that are not yet available to the general public |

What to expect after your surgery
You’ll work with your healthcare team to create a treatment plan tailored to your needs and preferences. There are several options for continuing your treatment after you have completed your first surgical resection. Be sure to communicate your treatment goals so your healthcare team can build them into the treatment plan.
Staying on track with follow-up care
Follow-up appointments, including imaging, are important for anyone managing glioma
These appointments are meant to help you and your doctor keep track of your treatment and how well it is working. Try to make time for your brain scan appointments when they are scheduled.
Your doctor may also assess your blood cells and your organ function and ask about possible side effects of your treatment. Certain changes in bodily function may require a smaller dose of medication or stopping treatment altogether for your safety. Your doctor may ask about new symptoms, your mental health, and how you’re doing day-to-day.
Brain scans can be stressful. It is not uncommon to feel nervous in the lead up to a scheduled scan and during the time that you are waiting to hear the result. Ask your care team how long it is likely to be before you can get the results and who you can contact to ask questions.
The follow-up appointments are usually more frequent in the beginning of your treatment and may become less so as time goes on. Follow-up appointments may differ from person to person, and depends on your treatment plan.

Advocating for yourself will help your doctor meet your treatment goals
You know your body better than anyone, so speak to your health care provider if you feel that something isn’t right.
The impact of glioma treatment on daily life
Depending on your treatment, whether it’s surgery, radiation therapy, or chemotherapy, you may experience side effects that impact your daily activities. It is important to keep track of these symptoms and report them to your care team if any become difficult to manage.
